Methadone is a very effective treatment, substantially tested by SAMHSA and other federal agencies as well as university. Still some doctors can do it wrong because they do not read up on the way the protocol is suppose to be administered. This is not a rare condition amongs mental health practitioners who often claims to be practicing, for example Cognitive Behavioral Therapy and the practitioners is not familiar with the research nor has ever taken a course in the use of the methodology. At best the practitioner may have read a book, but it is not totally familiar with all of what is suppose to be known. So often they practice the protocol wrong. Dr. B here gives us some ideas of how that might happen.
Recently I’ve had patients write to my blog describing how their opioid treatment program doctors are using methadone blood levels to determine the correct dose. What they described to me was worrisome; patients’ doses rarely need to be checked with methadone peak or trough blood levels. Due to tolerance, a methadone blood level may be adequate for one patient, but far too low for other patients.
A patient’s dose of methadone needs to be determined on clinical grounds. This can include the patient’s description of withdrawal symptoms and their timing related to dosing, physical exam just before the patient is due for a dose, and evaluation of the patient three to four hours after dosing. It may also include an evaluation of ongoing illicit opioid use, other medical issues, and other medication or illicit drug use.
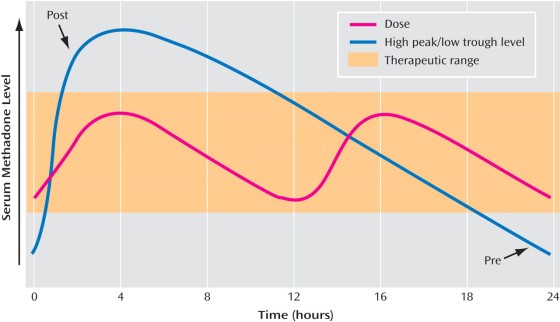
Opioid treatment program physicians rarely need to check methadone blood levels. I usually check peak and trough blood levels when I suspect a patient may be a fast metabolizer who may do better with split dosing. In such a case, the patient describes feeling fine for the first part of the day but in awful withdrawal by night time, despite taking a relatively higher dose. Then if the patient’s peak (highest level) is twice the trough (lowest level) I know they may feel better with twice a day dosing. Certain medications can induce the metabolism of methadone, making the patient metabolize methadone more quickly and drop the blood level. Often in this situation, split dosing helps.
I cringe when patients say things like, “my doctor checks a methadone blood level on everyone when they get to 80mg to see if they need to increase the dose or not.” For the vast majority of patients, getting this blood level won’t be helpful. If it’s used to determine the patient’s dose, it could be harmful. Many patients will still feel withdrawal while dosing at 80mg, even though they may have what would be considered a moderate blood level.
Our patients are tolerant to opioids. For this reason, methadone patients who are doing well, feel fine and have normal lives can have so-called “toxic” blood levels of methadone. A level that would kill someone unaccustomed to methadone may be just what my patient needs.
Some doctors think all opioid addicts want to go higher on their methadone dose than they need, and that these addicts would want limitless dose escalations unless the doctor stops this. In some patients, addiction may drive the addict to ask for dose increases even when not needed. Addiction often tells the patient “more is better.”
I’ve seen this problem too, but not as often as one might expect. More often, I’m the one advocating for a higher methadone dose. Don’t get me wrong, I do want to use the lowest effective dose. Some patients, due to fear of methadone and the stigma against it, are afraid to increase their dose. I point out that studies show patients do the best in methadone treatment if they are on a high enough dose to block the withdrawal symptoms and block the euphoria from other opioids. Particularly if the patient is still using illicit opioids, I recommend a dose increase.
Lab tests aren’t an adequate substitute for talking to the patient and examine the patient. As we used to say when I was in medical school, about a billion years ago, “Treat the patient, not the lab result.”
janaburson | April 19, 2015 at 1:56 pm | Tags: meethadone blood levels, methadone dose, methadone peak and trough | Categories: Methadone dosing | URL:http://wp.me/pT7TM-pw