Naloxone
Posted June 15, 2014 by janaburson in Families of Addicts and Alcoholics. Tagged: Harm reduction coalition,naloxone, Project Lazarus. 4 Comments
Medical journals, news outlets, and the internet have been exploding with new articles about naloxone. As awareness of this opioid overdose antidote grows, more people are pushing for this drug’s wider availability.
I’ve posted blogs about how the Project Lazarus kits have saved lives in my Appalachian corner of the world, but now let’s review some of the science behind naloxone.
Naloxone is an opioid antagonist, which means the drug binds to the mu opioid receptors in the brain, but instead of stimulating these receptors to produce euphoria and pain relief, naloxone does the opposite. It occupies the receptor and prevents opioids from attaching to these receptors to cause euphoria and pain relief. Naloxone has a high affinity to the mu opioid receptors, meaning it sticks like glue to them, but it does not activate these receptors.
If you give naloxone to an average person with no prior opioid use, not much will happen. Because naloxone can block our body’s own opioids, endorphins, that person might feel a little achy, tired, and irritable. But for the most part, when naloxone is given to a non-user of opioids, nothing happens.
If the patient has used opioids just once, recently, the patient won’t have withdrawal when given a dose of naloxone, since the body isn’t used to having opioids anyway. Naloxone in this case restores the body to its usual state. This’s why naloxone can be useful in a patient given opioids for surgical anesthesia. After the surgery is over, doctors can use naloxone to reverse the opioid anesthesia if they want the patient to wake up more quickly.
But in a patient with opioid addiction (or in a chronic pain patient) who uses opioids daily, naloxone causes opioid withdrawal. With long-standing opioid use, the body makes adjustments to counteract the chronic presence of opioids. When these opioids are whisked away with naloxone, this balance is abruptly upset, and the patient goes into precipitate withdrawal, if enough naloxone is given.
Naloxone is the opioid buzz-kill drug… and it’s also the opioid overdose life saver.
People die from opioid overdoses because the brain gets saturated with opioids. The part of the brain that tells us to breathe during sleep, the medulla, also gets saturated, and eventually shuts off. This usually occurs gradually. The respiratory rate slows over one to three hours, until all respirations stop. Then tissues of essential organs like the brain and heart die from lack of oxygen.
If naloxone can be given during this process, the opioids are tossed off brain receptors, and the medulla fires urgent orders for the body to resume breathing. The patient wakes up, so long as irreversible damage hasn’t yet been done to the brain and heart. In some cases, the patient goes into full precipitated opioid withdrawal, but usually the naloxone doesn’t reverse all of the opioids on board, just enough to save the patient’s life.
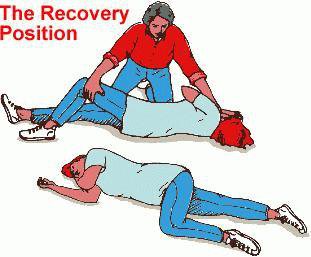
It’s a dramatic event. I’ve seen this in the emergency department during my Internal Medicine training. A patient can be lying on a stretcher, dead… then one dose of naloxone…. and they are sitting up, asking what happened to them. And sometimes they vomit. That’s another thing I learned in training. After giving a dose of naloxone, take one step back. Even better, place the patient in the “recovery position,” illustrated at the top of this blog, so that if they do vomit, they won’t aspirate the stuff into their lungs.
Naloxone is a relatively cheap drug, and it can be administered in several ways: intravenously, as doctors and EMS workers have always done, intramuscularly, subcutaneously, and intranasally.
Project Lazarus uses this last method. Their overdose kits contain two vials of naloxone 2mg each, and are in a syringe with a nozzle that is attached to the end of the syringe. This causes the medication to spray when the plunger of the syringe is pushed. It’s sprayed up in the nose of an unconscious person, and gets absorbed quickly. In fact, the response rates of all methods of naloxone administration are about the same – two to three minutes. If the patient doesn’t respond after a few minutes, the second dose can be given. Or if the patient initially responds but then gets sedated again, the second dose can be given.
The Harm Reduction Coalition gives out kits with a vial of naloxone and a 3cc syringe and needle. It takes some skill to administer naloxone intravenously, but this kit can be used intramuscularly or subcutaneously. All the rescuer has to do is draw the medication from the vial into the syringe, then stick the needle into the thigh muscle and push the plunger. Usually that delivers the medication into the muscle, unless the person has a great deal of fat between the skin and muscle. But that doesn’t matter, since this medication also works when injected into the subcutaneous tissue.
Each version of a naloxone kit has its advantages. The intranasal kit doesn’t require a needle, so there’s no risk of an accidental needle stick by the rescuer. But it’s a little more expensive. The intramuscular kits are really cheap, but some people in the community worry about handing out a needle and syringe that could be used to inject drugs. I don’t worry about that, since needle exchange should be done in every community, but that’s a bit of a tangent. More practically, addicts don’t use 3cc syringes; they’re too large. Addicts would miss their shot, and too much of their drug of abuse would get left behind in that big syringe.
I don’t think it matters what kind of kit is made available to addicts, their families, and first responders. We just need to get some kind of naloxone kit to these people.
Of course, all these kits contain the recommendation to call 911 immediately. But those precious minutes before EMS arrives may mean the difference between life and death. If naloxone can be given, the patient may be saved. Their brain function may be saved.
To be continued…