There is crisis in substance use treatment,a considerable sum of treatment approaches & methodology use by practitioners are not supported by Scientific Quantitative Empirical Research. Is it disconcerting that 72% of practitioners don’t read scientific articles in their field?(Butler, William & Wakefield,(1993)"Obstacle to disseminating Applied Psychological Science", Journal of Applied & Prevention Psychology2,for private comment you may email worsetreatmentihad@gmail.com
Saturday, August 8, 2015
http://www.aol.com/article/2015/08/07/hepatitis-increasingly-goes-hand-in-hand-with-heroin-abuse/21219975/?icid=maing-grid7%7Cmain5%7Cdl6%7Csec1_lnk3%26pLid%3D-1735803110
Hepatitis increasingly goes hand in hand with heroin abuse
PATRICK WHITTLE Aug 7th 2015 6:16PM
MACHIAS, Maine (AP) — Public health agencies and drug treatment centers nationwide are scrambling to battle an explosive increase in cases of hepatitis C, a scourge they believe stems at least in part from a surge in intravenous heroin use. In response, authorities are instituting or considering needle exchange programs but are often stymied by geography — many cases are in rural areas — and the cost of treatment in tight times.
In Washington County, at the nation's eastern edge, the rate of the acute form of hepatitis C last year was the highest in a state that was already more than triple the national average. The problem, health officials there agree, is spurred by the surge in the use of heroin and other injectable drugs and the sharing of needles to get high.
Ryan Kinsella's story is sadly typical. He was badly hurt in a rock climbing accident and became dependent on opioid painkillers several years ago. But when his prescriptions ran out, he sought drugs from the street, where he found heroin cheaper and easy to get, replacing one addiction for another. He's now recovering from hepatitis C.
"It's tough getting medical professionals to look at you as something that's not a junkie," said Kinsella, 33, who runs a bicycle shop in tiny Penobscot, next door in Hancock County. "There's a little bit of social stigma, and there's a little bit of 'There's nothing we can do for you' that's hard to hear." Maine is undergoing its worst outbreak of acute hepatitis C since it started to record cases in the 1990s. In Washington County, the rate is about 6 cases per 100,000 residents, well above the national rate of about 0.7 per 100,000. But the problem is not limited to Maine, by far. It has afflicted other areas where heroin use is a growing concern, such as:
— Springfield, Missouri, where the disease is on the rise and police have already confiscated more than five times the amount of heroin as in 2013.
— Madison County, Indiana, which had 70 new cases of hepatitis C in 2013, followed by 130 in 2014, and where health officials expect current rates to at least match or surpass last year's. (Indiana's Scott County is also grappling with an HIV outbreak among injection drug users.)
— Massachusetts, where cases of acute hepatitis C grew from 10 in 2009 to 174 in 2013.
— Large swaths of Appalachia. Kentucky leads the nation in the rate of acute hepatitis C, with 5.1 cases for every 100,000 residents, more than seven times the national average, according to 2013 data from the Centers for Disease Control and Prevention. Hepatitis C, which can result in liver failure, liver cancer and other serious complications, is the nation's most common blood-borne infection. About 3 million Americans are infected, according to federal statistics. It presents as either acute, or short-term, and chronic, which can last a lifetime. Both forms are most closely linked to needle-sharing, although hepatitis C is less commonly spread through unprotected sex or other contact with infected blood.
Nationwide, the number of cases of acute hepatitis C grew 273 percent from 2009 to 2013, the CDC reported in its most recently available statistics. Tracking similarly is heroin use; the CDC reported that the number of users nationwide rose nearly 150 percent from 2007 to 2013 and that use of the drug also more than doubled among ages 18 to 25 in the decade that ended in 2013.
More than 19,000 people died from hepatitis C in 2013, up from 16,235 in 2009, according to the CDC. Although the agency hasn't established a causal link between individual hepatitis C outbreaks and injected drug use, it notes that injected drug use is the primary risk factor for hepatitis C infection in this country.
Many local health agencies and health care providers have made the connection or are confident there is one, and are allowing users to turn in dirty syringes in exchange for clean ones. But many states disallow the practice and federal funding for it is banned. Madison County, in central Indiana, won approval in June to run a needle-exchange program to fight the spread of hepatitis C among intravenous drug users. Clallam County, Washington, public health program manager Christina Hurst operates the local needle exchange program and calls it "one of the best interventions we have for this prevention," and a key tool to prevent dirty needles from being discarded in public. A rise in acute hepatitis C, which nearly tripled in Washington between 2009 and 2013, is due to "most likely the needle sharing aspect of needle drug use," Hurst said. Maine's Downeast AIDS Network opened the only needle exchange program in Washington County about a year ago in Machias, the county seat, one of six such programs in the mostly rural state.
The AIDS Resource Center of Wisconsin, which also provides services for people with hepatitis, says it collected more than 3 million needles in 2014, up from a million in 2010.
Last month, a law took effect in Ohio making it easier for health departments to establish needle exchanges. The state had more than 100 cases of acute hepatitis C last year and the previous year, up from single digits in 2005 and 2006. In Franklin County, home to Columbus, the capital and the state's largest city, hepatitis C was diagnosed in 1,369 people last year, up from 719 in 2010. A decade ago, it had zero cases.
The costs of prevention and treatment often fall on public health agencies when many patients don't have insurance and can't pay. That can add up fast when just getting a diagnosis can be $19, said Scott Stokes, executive director of the Wisconsin AIDS center.
Rural regions like Washington County and parts of Appalachia and the Midwest struggle with drug problems because of poverty, job shortages and the difficulty of providing care in a vast area with few large population centers, said Kenney Miller, executive director of the Downeast AIDS Network.
The virus differs from hepatitis A, which is spread person-to-person or via contaminated food or water, and hepatitis B, which is transmitted by bodily fluids. There are vaccines for hepatitis A and B, unlike hepatitis C, for which there is none.
New treatments are available, but they're expensive and out of reach of most of the rural poor who make up the ranks of the infected. For instance, Harvoni, the leading drug to treat hepatitis C, costs more than $1,300 per pill.
Even so, the number of prescriptions filled for hepatitis C drugs more than doubled to a monthly average of 48,000 during the early part of 2015.
___
Associated Press writer Andrew Welsh-Huggins in Columbus, Ohio, and AP Medical Writer Mike Stobbe in New York contributed to this report.
Hepatitis increasingly goes hand in hand with heroin abuse
PATRICK WHITTLE Aug 7th 2015 6:16PM
MACHIAS, Maine (AP) — Public health agencies and drug treatment centers nationwide are scrambling to battle an explosive increase in cases of hepatitis C, a scourge they believe stems at least in part from a surge in intravenous heroin use. In response, authorities are instituting or considering needle exchange programs but are often stymied by geography — many cases are in rural areas — and the cost of treatment in tight times.
In Washington County, at the nation's eastern edge, the rate of the acute form of hepatitis C last year was the highest in a state that was already more than triple the national average. The problem, health officials there agree, is spurred by the surge in the use of heroin and other injectable drugs and the sharing of needles to get high.
Ryan Kinsella's story is sadly typical. He was badly hurt in a rock climbing accident and became dependent on opioid painkillers several years ago. But when his prescriptions ran out, he sought drugs from the street, where he found heroin cheaper and easy to get, replacing one addiction for another. He's now recovering from hepatitis C.
"It's tough getting medical professionals to look at you as something that's not a junkie," said Kinsella, 33, who runs a bicycle shop in tiny Penobscot, next door in Hancock County. "There's a little bit of social stigma, and there's a little bit of 'There's nothing we can do for you' that's hard to hear." Maine is undergoing its worst outbreak of acute hepatitis C since it started to record cases in the 1990s. In Washington County, the rate is about 6 cases per 100,000 residents, well above the national rate of about 0.7 per 100,000. But the problem is not limited to Maine, by far. It has afflicted other areas where heroin use is a growing concern, such as:
— Springfield, Missouri, where the disease is on the rise and police have already confiscated more than five times the amount of heroin as in 2013.
— Madison County, Indiana, which had 70 new cases of hepatitis C in 2013, followed by 130 in 2014, and where health officials expect current rates to at least match or surpass last year's. (Indiana's Scott County is also grappling with an HIV outbreak among injection drug users.)
— Massachusetts, where cases of acute hepatitis C grew from 10 in 2009 to 174 in 2013.
— Large swaths of Appalachia. Kentucky leads the nation in the rate of acute hepatitis C, with 5.1 cases for every 100,000 residents, more than seven times the national average, according to 2013 data from the Centers for Disease Control and Prevention. Hepatitis C, which can result in liver failure, liver cancer and other serious complications, is the nation's most common blood-borne infection. About 3 million Americans are infected, according to federal statistics. It presents as either acute, or short-term, and chronic, which can last a lifetime. Both forms are most closely linked to needle-sharing, although hepatitis C is less commonly spread through unprotected sex or other contact with infected blood.
Nationwide, the number of cases of acute hepatitis C grew 273 percent from 2009 to 2013, the CDC reported in its most recently available statistics. Tracking similarly is heroin use; the CDC reported that the number of users nationwide rose nearly 150 percent from 2007 to 2013 and that use of the drug also more than doubled among ages 18 to 25 in the decade that ended in 2013.
More than 19,000 people died from hepatitis C in 2013, up from 16,235 in 2009, according to the CDC. Although the agency hasn't established a causal link between individual hepatitis C outbreaks and injected drug use, it notes that injected drug use is the primary risk factor for hepatitis C infection in this country.
Many local health agencies and health care providers have made the connection or are confident there is one, and are allowing users to turn in dirty syringes in exchange for clean ones. But many states disallow the practice and federal funding for it is banned. Madison County, in central Indiana, won approval in June to run a needle-exchange program to fight the spread of hepatitis C among intravenous drug users. Clallam County, Washington, public health program manager Christina Hurst operates the local needle exchange program and calls it "one of the best interventions we have for this prevention," and a key tool to prevent dirty needles from being discarded in public. A rise in acute hepatitis C, which nearly tripled in Washington between 2009 and 2013, is due to "most likely the needle sharing aspect of needle drug use," Hurst said. Maine's Downeast AIDS Network opened the only needle exchange program in Washington County about a year ago in Machias, the county seat, one of six such programs in the mostly rural state.
The AIDS Resource Center of Wisconsin, which also provides services for people with hepatitis, says it collected more than 3 million needles in 2014, up from a million in 2010.
Last month, a law took effect in Ohio making it easier for health departments to establish needle exchanges. The state had more than 100 cases of acute hepatitis C last year and the previous year, up from single digits in 2005 and 2006. In Franklin County, home to Columbus, the capital and the state's largest city, hepatitis C was diagnosed in 1,369 people last year, up from 719 in 2010. A decade ago, it had zero cases.
The costs of prevention and treatment often fall on public health agencies when many patients don't have insurance and can't pay. That can add up fast when just getting a diagnosis can be $19, said Scott Stokes, executive director of the Wisconsin AIDS center.
Rural regions like Washington County and parts of Appalachia and the Midwest struggle with drug problems because of poverty, job shortages and the difficulty of providing care in a vast area with few large population centers, said Kenney Miller, executive director of the Downeast AIDS Network.
The virus differs from hepatitis A, which is spread person-to-person or via contaminated food or water, and hepatitis B, which is transmitted by bodily fluids. There are vaccines for hepatitis A and B, unlike hepatitis C, for which there is none.
New treatments are available, but they're expensive and out of reach of most of the rural poor who make up the ranks of the infected. For instance, Harvoni, the leading drug to treat hepatitis C, costs more than $1,300 per pill.
Even so, the number of prescriptions filled for hepatitis C drugs more than doubled to a monthly average of 48,000 during the early part of 2015.
___
Associated Press writer Andrew Welsh-Huggins in Columbus, Ohio, and AP Medical Writer Mike Stobbe in New York contributed to this report.
Saturday, August 1, 2015
This is a meeting of the South Florida Center for Independent Living and organization that deals with people with physical or mental disabilities or impairments. They are calling for the help that they may offer businesses in our community to make services available.
Am concern that we should make people aware of the problems that exist in the mental health but specially in the substance use treatment facilities. Abuses and lack of real treatment.
Am concern that we should make people aware of the problems that exist in the mental health but specially in the substance use treatment facilities. Abuses and lack of real treatment.
You're invited to the meeting of the
|
Disability Advocacy Council of the Center for Independent Living of South Florida
|
Are you a business owner interested in learning how you can be disability-friendly? Do you want to know when a sign language interpreter is required, and when it is not? Are you interested in learning about service dogs? Do you want to learn about what a business is required to do under the Americans With Disabilities Act?
Are you an individual with a disability, or, a caregiver? Do you want information about emergency shelters and services to evacuees with disabilities? Do you have questions and concerns about the Florida Medicaid Managed Care Program? Do you have concerns about Special Transportation Services?
On Thursday, August 6, 2015, from 10:00 a.m. to 12:00 Noon, Marc Dubin, Director of Advocacy, will moderate a discussion at the Center for Independent Living of South Florida, Inc., 6660 Biscayne Boulevard, Miami, FL 33138. Free parking is located behind the building. Marc is an expert in the ADA, having served as a Sr. Trial Attorney at the Justice Dept., in the Disability Rights Section of the Civil Rights Division. In that capacity, he provided education about the ADA nationwide, and enforced the ADA nationwide, on behalf of the United States.
If you are unable to attend in person, our toll free conference line is available. Please call (866) 730-7514, Conference Pin 938460# on the morning of the meeting.
Subscribe to our ADA Expertise Listserve and receive information directly to your inbox. To subscribe, Email Marc Dubin, Esq., at Email: mdubin@pobox.com. In the subject line write "Subscribe to ADA Listserve."
|
When
|
THURSDAY
August 6, 2015 10:00 a.m. -- 12:00 Noon |
Where
|
Center for Independent Living
of South Florida
6660 Biscayne Boulevard
Miami, FL 33138
|
Thursday, May 14, 2015
The BUSINESS of Recovery
A Review: The Business of Recovery
POSTED ON APRIL 2, 2015
A documentary film directed by Adam Finberg and produced by Greg Horvath | Review by Tom Horvath, Ph.D.
 What do you really know about the addiction rehab industry?
What do you really know about the addiction rehab industry?
Like most people, you may be under the impression that addiction treatment is a life-saving, highly ethical enterprise, with services provided by highly trained professionals. You might also think these professionals utilize addiction treatment methods based on the latest scientific research and hold themselves accountable to the highest standards. If so, you will likely have a very different perspective after you see this film.
The Business of Recovery is a must-see film for every one of us. In the US alone, more than 2/3 of families have been touched by addiction and over two million people enter some level of addiction treatment each year. None of us are immune. This issue will affect you and someone you care about. You need to be informed.
Overview
This film follows the true story of several individuals and their families as they embark on their journey to recovery. It reveals their experiences in addiction treatment and includes interviews with multiple treatment “experts” connected to the 35 billion dollar treatment industry. The contrast between the expert statements and the truth is dramatic. The experiences and outcomes of treatment for the individuals interviewed are far less than ideal. The Business of Recovery reveals the extremely low ethical standards of the rehab industry and the truth behind the many unlicensed and unprofessional individuals who run it. The unfortunate reality is that vulnerable families who are seeking help for a loved one in crisis are being met with high-pressure sales tactics rather than compassionate care and reliable information. The self-interest of the addiction treatment industry is shockingly apparent. Be prepared: The client stories in this film are infuriating and heartbreaking.
Mission
The mission behind The Business of Recovery is to educate the public and bring about change. The public needs to demand: 1) better government regulations and oversight, 2) science based treatments, and 3) a higher level of education for those who treat addiction. Scientifically based addiction treatment does exist. However, many US treatment facilities appear to operate largely in isolation from this body of scientific work. Unbelievably, several high profile treatment industry leaders interviewed in this film appear to be unaware of this science. Since the 1980’s, scientific reviewers have suggested that the US addiction treatment system appears to be based on treatments that have the least evidence of effectiveness. This film reveals that decades later the situation has not changed. Although critics of US addiction treatment have been aware of this situation for many years, few in the general public appear to be aware of it—until now.
I hope this film leads to public outrage about the addiction treatment industry. It is also my hope that this film creates more sophisticated consumers of rehab services and provides an impetus to improvements in government regulation and overall standards within the addiction treatment industry. The process of getting to these outcomes will be tedious and tumultuous. Many individuals may leave the field or lose their jobs, and many organizations will need to radically re-shape themselves or cease to exist. Nevertheless, these changes are long overdue.
A sneak preview of The Business of Recovery was shown to a packed audience on March 27, 2015, at the Phoenix Film Festival. The official world premiere was April 26 at the Newport Beach Film Festival.
Disclaimer: Dr. Tom Horvath, the author of this piece, was interviewed extensively for this film, both on and off camera. A small portion of his on-camera interview is included in the film. His company, Practical Recovery, operates two inpatient rehabs, anoutpatient rehab and provides sober living and detox services. It is his belief that it is possible to provide addiction treatment in a responsible, ethical and transparent manner. The producer of the film, Greg Horvath, is unrelated to the author.
Monday, April 20, 2015
You see what I mean, even effective treatment can be done wrong
Methadone is a very effective treatment, substantially tested by SAMHSA and other federal agencies as well as university. Still some doctors can do it wrong because they do not read up on the way the protocol is suppose to be administered. This is not a rare condition amongs mental health practitioners who often claims to be practicing, for example Cognitive Behavioral Therapy and the practitioners is not familiar with the research nor has ever taken a course in the use of the methodology. At best the practitioner may have read a book, but it is not totally familiar with all of what is suppose to be known. So often they practice the protocol wrong. Dr. B here gives us some ideas of how that might happen.
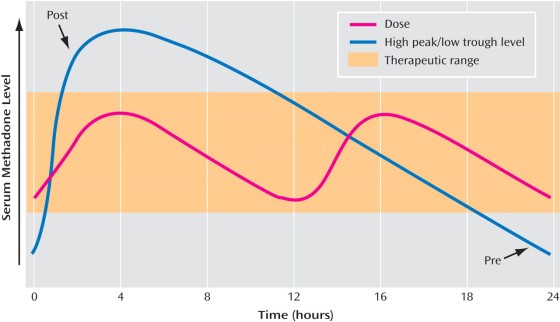
Recently I’ve had patients write to my blog describing how their opioid treatment program doctors are using methadone blood levels to determine the correct dose. What they described to me was worrisome; patients’ doses rarely need to be checked with methadone peak or trough blood levels. Due to tolerance, a methadone blood level may be adequate for one patient, but far too low for other patients.
A patient’s dose of methadone needs to be determined on clinical grounds. This can include the patient’s description of withdrawal symptoms and their timing related to dosing, physical exam just before the patient is due for a dose, and evaluation of the patient three to four hours after dosing. It may also include an evaluation of ongoing illicit opioid use, other medical issues, and other medication or illicit drug use.
Opioid treatment program physicians rarely need to check methadone blood levels. I usually check peak and trough blood levels when I suspect a patient may be a fast metabolizer who may do better with split dosing. In such a case, the patient describes feeling fine for the first part of the day but in awful withdrawal by night time, despite taking a relatively higher dose. Then if the patient’s peak (highest level) is twice the trough (lowest level) I know they may feel better with twice a day dosing. Certain medications can induce the metabolism of methadone, making the patient metabolize methadone more quickly and drop the blood level. Often in this situation, split dosing helps.
I cringe when patients say things like, “my doctor checks a methadone blood level on everyone when they get to 80mg to see if they need to increase the dose or not.” For the vast majority of patients, getting this blood level won’t be helpful. If it’s used to determine the patient’s dose, it could be harmful. Many patients will still feel withdrawal while dosing at 80mg, even though they may have what would be considered a moderate blood level.
Our patients are tolerant to opioids. For this reason, methadone patients who are doing well, feel fine and have normal lives can have so-called “toxic” blood levels of methadone. A level that would kill someone unaccustomed to methadone may be just what my patient needs.
Some doctors think all opioid addicts want to go higher on their methadone dose than they need, and that these addicts would want limitless dose escalations unless the doctor stops this. In some patients, addiction may drive the addict to ask for dose increases even when not needed. Addiction often tells the patient “more is better.”
I’ve seen this problem too, but not as often as one might expect. More often, I’m the one advocating for a higher methadone dose. Don’t get me wrong, I do want to use the lowest effective dose. Some patients, due to fear of methadone and the stigma against it, are afraid to increase their dose. I point out that studies show patients do the best in methadone treatment if they are on a high enough dose to block the withdrawal symptoms and block the euphoria from other opioids. Particularly if the patient is still using illicit opioids, I recommend a dose increase.
Lab tests aren’t an adequate substitute for talking to the patient and examine the patient. As we used to say when I was in medical school, about a billion years ago, “Treat the patient, not the lab result.”
janaburson | April 19, 2015 at 1:56 pm | Tags: meethadone blood levels, methadone dose, methadone peak and trough | Categories: Methadone dosing | URL:http://wp.me/pT7TM-pw
Friday, April 17, 2015
What? Methadone and Suboxone is Substance Use Medical Treatment
Methadone patients need not to apologist.
Here is a treatment for Opiate 'Addiction' that have highly criticize and consider controversial by the 12 Step and most abstinent based residential rehabilitation facilities. Of course most of these people who criticize these medically assisted recovery are science illiterates who wouldn't no the difference between efficiency and safety and what really does not work. They do not know about Confirmation Bias http://en.wikipedia.org/wiki/Confirmation_bias the basic reason why we need to do research. You see when you think you know something for sure that gets in the way of discovery and exploration. An attitude require for most scientific oriented minds. Most doctors practice discovery or looking for the reason of your ailments or symptoms. Correlation Illusion http://en.wikipedia.org/wiki/Illusory_correlation is another reason why research is necessary. You see most of these individuals and a substantial amount of professionals in mental health practice and make claims which are based on Face value (or Validity http://en.wikipedia.org/wiki/Face_validity
Most people operate on the illusion that because it appears to be a good idea or a claim seem to be true, it most be true. Although this is so sometimes, it is not all of the time. Face value is good to develop hypothesis to be tested but by itself has a lot of room for error and in fact it is frequently
Clinical judgment in psychology and mental health is frequently inaccurate, in fact too many are right down faliable
The lack of science and ignoring evidence based treatment is keeping mental health and substance use in the stone age.
No body cares about alcoholics and drug addicts. Enough misinformation is enough
There are tons of science based information, why is it being ignored by mainstream mental health and substance use treatment staff. I believe that when treatment is not based on medical science. Other types of treatment that has never been proven to be effective and safe is considered malpractice. In the law of torts, malpractice is an "instance of negligence or incompetence on the part of a professional". In fact most of these science based information is published by the federal government, yet the public and potential patients are missing the facts because it is not being provided.
The State Methadone Treatment Guidelines were first printed and published in 1993. The methadone treatment facilities ran by Miami Dade Office of Rehabilitation Services were oblivious of its existence. when I brought it to their attention the supervisors response was "Oh, they are only guidelines" obviously he most have thought that the ignorance of science is bliss. Eventually, Miami DADE COUNTY ORS finally stopped providing this type of treatment in favor of the religious indoctrination of alcoholics anonymous. A program that when it was first implemented in the late 1970 and 80 had not been tested for effectiveness and safety (read Why Bogus Treatment appears to work. A problem that is widely connected with mental health and substance use treatment.
http://www.ctcertboard.org/files/TIP1.pdf
Why Bogus Treatment Appears to Work
http://www.csicop.org/si/show/why_bogus_therapies_seem_to_work/
Why are attorneys missing out on this area of malpractice can only be because they are just as prejudice, and bigots.
Here is a treatment that is outright effective and safe and seems like patients have to beg and hope that they will be accepted.
THE ARE NO REASON FOR ANY METHADONE OR SUBOXONE PATIENT TO BE APOLOGETIC. THIS TREATMENT WORKS AND IMPROVE PEOPLE LIFE.
Original article appeared in:
Here is a treatment for Opiate 'Addiction' that have highly criticize and consider controversial by the 12 Step and most abstinent based residential rehabilitation facilities. Of course most of these people who criticize these medically assisted recovery are science illiterates who wouldn't no the difference between efficiency and safety and what really does not work. They do not know about Confirmation Bias http://en.wikipedia.org/wiki/Confirmation_bias the basic reason why we need to do research. You see when you think you know something for sure that gets in the way of discovery and exploration. An attitude require for most scientific oriented minds. Most doctors practice discovery or looking for the reason of your ailments or symptoms. Correlation Illusion http://en.wikipedia.org/wiki/Illusory_correlation is another reason why research is necessary. You see most of these individuals and a substantial amount of professionals in mental health practice and make claims which are based on Face value (or Validity http://en.wikipedia.org/wiki/Face_validity
Most people operate on the illusion that because it appears to be a good idea or a claim seem to be true, it most be true. Although this is so sometimes, it is not all of the time. Face value is good to develop hypothesis to be tested but by itself has a lot of room for error and in fact it is frequently
Clinical judgment in psychology and mental health is frequently inaccurate, in fact too many are right down faliable
The lack of science and ignoring evidence based treatment is keeping mental health and substance use in the stone age.
No body cares about alcoholics and drug addicts. Enough misinformation is enough
There are tons of science based information, why is it being ignored by mainstream mental health and substance use treatment staff. I believe that when treatment is not based on medical science. Other types of treatment that has never been proven to be effective and safe is considered malpractice. In the law of torts, malpractice is an "instance of negligence or incompetence on the part of a professional". In fact most of these science based information is published by the federal government, yet the public and potential patients are missing the facts because it is not being provided.
The State Methadone Treatment Guidelines were first printed and published in 1993. The methadone treatment facilities ran by Miami Dade Office of Rehabilitation Services were oblivious of its existence. when I brought it to their attention the supervisors response was "Oh, they are only guidelines" obviously he most have thought that the ignorance of science is bliss. Eventually, Miami DADE COUNTY ORS finally stopped providing this type of treatment in favor of the religious indoctrination of alcoholics anonymous. A program that when it was first implemented in the late 1970 and 80 had not been tested for effectiveness and safety (read Why Bogus Treatment appears to work. A problem that is widely connected with mental health and substance use treatment.
http://www.ctcertboard.org/files/TIP1.pdf
Why Bogus Treatment Appears to Work
http://www.csicop.org/si/show/why_bogus_therapies_seem_to_work/
Why are attorneys missing out on this area of malpractice can only be because they are just as prejudice, and bigots.
Here is a treatment that is outright effective and safe and seems like patients have to beg and hope that they will be accepted.
THE ARE NO REASON FOR ANY METHADONE OR SUBOXONE PATIENT TO BE APOLOGETIC. THIS TREATMENT WORKS AND IMPROVE PEOPLE LIFE.
Original article appeared in:
Methadone and Buprenorphine 101: A Guide for Law Enforcement
Posted: 04/15/2015 10:41 am EDT Updated: 04/15/2015 10:59 am EDT
Lately, with all the talk about rising rates of opioid use and addiction, we are hearing more about opioid treatment programs (OTPs). OTPs provide opioid-dependent patients with behavioral therapy and medication, such as methadone or Suboxone (buprenorphine), sometimes called medication assisted therapy, (MAT), to control cravings for illicit opioids and help them resume normal lives. Although opioid treatment programs have been around for decades with verified results, information about these programs can be confusing for members of law enforcement and communities. Do these medications cause driving impairment? How do OTPs affect the criminal justice system? What safeguards are in place to prevent abuse?
To get some answers, I spoke with Tad Clodfelter, PsyD, President and CEO of SouthLight Healthcare in Raleigh, North Carolina. SouthLight provides behavioral health care and treatment for addiction and mental illness, including methadone and buprenorphine (Suboxone) treatment for opioid dependence. Here are some of his answers to law enforcement FAQs on opioid treatment programs.
What are OTPs?
Opioid treatment programs (OTPs) combine behavioral care services with the delivery of medications that help control cravings for opioids. OTPs are the only FDA recommended treatment for opioid dependence. They are historically equated with methadone treatment, but over the past 5-10 years these programs have evolved to include other methods of medication assisted treatment (MAT), such as Suboxone (buprenorphine).
What is the difference between methadone and Suboxone?
Suboxone and Methadone are both synthetic opioids and used to treat patients with opioid dependency or addiction; however, they are not necessarily used interchangeably, and there are differences in their effects. Methadone is a full opioid agonist, which means it binds to opioid receptors in the brain to take away the physiological cravings for opioid drugs and abuse, allowing the person to function well in their day-to-day lives without being intoxicated, hold down a job and reclaim their families. Methadone is typically given to persons with heavy opiate habits. Suboxone is a partial agonist that affords similar results, also allowing people to resume normal lives. Different people respond better to one versus the other of these effective medications.
Can OTP medications be abused?
Methadone and Suboxone can be abused and diverted, but are far less likely to be than street opioids or prescription pain medications. OTPs have tight restrictions to limit the likelihood of diversion. SouthLight has a good track record of preventing abuse, as do many reputable clinics.
Methadone and Suboxone can be abused and diverted, but are far less likely to be than street opioids or prescription pain medications. OTPs have tight restrictions to limit the likelihood of diversion. SouthLight has a good track record of preventing abuse, as do many reputable clinics.
What are the safeguards in place to prevent diversion and abuse?
At Suboxone clinics the staff do pill counts. Sometimes they have patients come back to the clinic and bring in their pills, which are counted to make sure the patient hasn't taken more than their prescribed dose. With methadone, the patients come to the treatment facility daily to receive their dose under staff supervision. Once they have demonstrated commitment to the program and established a good track record, they earn the privilege of taking home medication in a locked box. The person is mandated to return the medication any time there is any suspicion or concern that they might be abusing it. OTPs check for suspicious behavior using urine drug testing, observing any changes in behavior, and checking the Controlled Substance Reporting System to see if the person might be getting other prescriptions from doctors that might be a concern. A person can qualify for take-home doses after 3 months, but that privilege can be taken away for noncompliance.
Do OTP medications cause driving impairment?
Not when taken as prescribed. Someone leaving a methadone or Suboxone clinic who has just taken their normal dose should not have trouble driving. In a clinic setting, patients are observed closely. A patient is not allowed to leave the clinic if a concern, i.e., intoxication, ever exists.
Do OTPs just substitute one addiction for another?
No. Methadone or Suboxone is essential in opioid treatment. These medications, in combination with evidence-based behavioral therapies, are the FDA-recommended standards of care for opioid dependence. In essence, medication assisted therapy substitutes a controlled synthetic opiate for opiate drugs of abuse. The scientific, medical literature is clear in recommending these treatments for opioid dependence. Why? Sustained or long-term opiate use chemically alters the brain and negatively impacts the sensitivity of the body's opioid receptors. In order to begin the recovery process from opioid addiction, medication assisted or replacement therapy is critical to healing the brain and body. Further, the number of opioid dependent persons who can successfully quit drug use "cold turkey" is extremely low due to intense cravings and withdrawal symptoms, which are part of the opioid dependence syndrome. MAT is used to sustain a person and prevent relapse as well.
At SouthLight Healthcare, we serve 400 people at any given time and have a good track record of solid results during and after treatment. The standard of care works very well if treatment regimens are adhered to by patients. Of course, treatment doesn't work flawlessly in every case, but neither does treatment for any chronic, relapsing disease, which substance dependence is. As such, opioid dependence, like other chronic, relapsing medical disorders, requires a combination of treatments, including medication and behavioral modification or change, in order to achieve impactful and sustained treatment results.
What are some of the benefits of OTPs for patients and the community?
OTPs benefit the communities they serve in tremendous and deep reaching ways, many of which are below the radar. They are real and tangible. The vast majority of our clients are in the workforce with documented jobs, paying taxes and giving back to the community. When people are in treatment and stable and reclaiming or simply living their lives, jobs and families, they are less likely to encounter the criminal justice system. That is a major cost savings to society. Our jails are filled with people who are addicted or mentally ill or both; many have committed nonviolent crimes. Such citizens are better served by treatment, which helps them to mend relationships and realize professional goals - the things that makes life worth living.
OTPs benefit the communities they serve in tremendous and deep reaching ways, many of which are below the radar. They are real and tangible. The vast majority of our clients are in the workforce with documented jobs, paying taxes and giving back to the community. When people are in treatment and stable and reclaiming or simply living their lives, jobs and families, they are less likely to encounter the criminal justice system. That is a major cost savings to society. Our jails are filled with people who are addicted or mentally ill or both; many have committed nonviolent crimes. Such citizens are better served by treatment, which helps them to mend relationships and realize professional goals - the things that makes life worth living.
The Centers for Disease Control (CDC) lists the following benefits of methadone treatment (MMT): http://www.cdc.gov/idu/facts/MethadoneFin.pdf
• reduced or stopped use of injection drugs;
• reduced risk of overdose and of acquiring or transmitting diseases such as HIV, hepatitis B or C, bacterial infections, endocarditis, soft tissue infections, thrombophlebitis, tuberculosis, and STDs;
• reduced mortality - the median death rate of opiate-dependent individuals in MMT is 30 percent of the rate of those not in MMT;
• possible reduction in sexual risk behaviors, although evidence on this point is conflicting;
• reduced criminal activity;
• improved family stability and employment potential; and
• improved pregnancy outcomes.
• reduced risk of overdose and of acquiring or transmitting diseases such as HIV, hepatitis B or C, bacterial infections, endocarditis, soft tissue infections, thrombophlebitis, tuberculosis, and STDs;
• reduced mortality - the median death rate of opiate-dependent individuals in MMT is 30 percent of the rate of those not in MMT;
• possible reduction in sexual risk behaviors, although evidence on this point is conflicting;
• reduced criminal activity;
• improved family stability and employment potential; and
• improved pregnancy outcomes.
Cost savings
• the annual costs of methadone maintenance treatment are much lower than the annual costs of either untreated heroin use, incarceration or drug-free treatment programs
• criminal activities related to heroin use resulted in social costs that were four times higher than the cost of methadone maintenance treatment;http://www.chodarr.org/node/1398
• for every dollar spent on methadone maintenance treatment there is a savings to the community of between US$4-$13.
• the annual costs of methadone maintenance treatment are much lower than the annual costs of either untreated heroin use, incarceration or drug-free treatment programs
• criminal activities related to heroin use resulted in social costs that were four times higher than the cost of methadone maintenance treatment;http://www.chodarr.org/node/1398
• for every dollar spent on methadone maintenance treatment there is a savings to the community of between US$4-$13.
This service is being provided by the South FLORIDA Chapter of NAMA National Alliance for Medication Assisted Recovery
at http://www.methadone.org
Tuesday, April 14, 2015
The Stigma Must Stop
Anti-drug czar: 'Every life is worth saving'
COVINGTON – The stigma of drug addiction, the stigma of using medicine to treat it, the stigma of needle exchange and the idea that a life-saving drug shouldn't be used for overdose victims all need to end.
Michael Botticelli, the director of White House Office of National Drug Control Policy, delivered these messages when he visited Northern Kentucky on Thursday.
Botticelli made it clear while at the Metropolitan Club in Covington at the invitation of the Northern Kentucky Chamber of Commerce that he is in favor of using naloxone to save lives. The non-narcotic blocks the effects of heroin or prescription painkillers and can restore breathing in overdose victims.
"Every life is worth saving," Botticelli told an audience member who questioned whether the drug enables addicts to continue to use heroin. He added that there is no indication that drug addicts will feel safer using heroin because they have access to naloxone.
Botticelli urged a holistic approach, providing both prevention lessons to young children and families and using every treatment and counseling option to help addicts.
He lauded the Northern Kentucky Chamber of Commerce's efforts in the regional heroin fight saying he knows of no other chamber in the nation that has stepped forward to help manage the crisis.
U.S. Sen. Mitch McConnell, R-Ky., said he brought Botticelli to the region to learn about its plight with the opioid and heroin epidemic that is plaguing the nation and, particularly, coursing through Northern Kentucky.
"I am here with the director of drug control policy (appointed by President Barack Obama) because this is beyond partisan debate," the Senate majority leader told chamber members, families advocating recovery, treatment and public health officials at the event.
Listing statistic after statistic, from the tripling of St. Elizabeth Healthcare's emergency care of overdose victims since 2011 to Kentucky's 1,049 lost lives to overdoses in 2013, McConnell said, "In Northern Kentucky, we're at the epicenter" of the crisis with heroin and prescription painkiller addiction.
Earlier in the day, Botticelli was given a private tour of St. Elizabeth Healthcare – Edgewood, where he visited the Neonatal Intensive Care Unit to see newborns with Neonatal Abstinence Syndrome. He heard from Dr. Lynn Saddler, director of the Northern Kentucky Health Department; Jason Merrick, chairman of Northern Kentucky People Advocating Recover; Bonnie Hedrick, coordinator of the NKY Prevention Alliance and others who have joined in the local fight against heroin.
They said Botticelli offered ideas on how they can tap into federal funds available for community substance abuse prevention and support.
In an exclusive interview with The Enquirer, Botticelli said drug courts, treatment centers and corrections systems need to provide medicine assisted treatment, and not just abstinence programs.
"Evidence is strikingly clear that people with opioid disorder do remarkably better with medication assisted treatment – along with counseling," Botticelli told The Enquirer. "It's our hope that medication assisted treatment is the standard of care."
Toward that end, the anti-drug czar said, his office has changed its policy – and has made the inclusion of medicine assisted treatment a condition for state drug courts to receive federal funds.
Kentucky has come under criticism because its drug courts – with the exception of Pulaski County's – require abstinence. Judges even require addicts who have been prescribed medicine for their addiction to taper off of it as a condition of remaining in drug court. But Northern Kentucky drug courts are primarily funded by the state. Only a few counties – none in Northern Kentucky – use federal funds, and that is for training, according to the Kentucky Administrative Office of the Courts.
Botticelli said the federal government is also urging treatment centers to use "every option" available to treat those with addiction, and noted that for opioid and heroin addicts, scientific evidence shows medicine-assisted treatment often works best.
Kimberly Wright of Cold Spring, an activist in the heroin fight and mother of a daughter who is a recovering heroin addict, said she hopes that Kentucky listens to the message.
"We need medicine assisted treatment in Kentucky drug courts. We need an overhaul of our rehabs (to include it)," Wright said.
Joan Arlinghaus, a member of NKY People Advocating Recovery, believes Botticelli's visit was valuable for the region.
"I think it will raise a lot of awareness," she said, "and erase some of the stigma that comes with addiction."
Monday, March 2, 2015
Why Bogus Therapies Seem to Work.
Most treatment in mental health but specifically in Substance Use is totally created from hunches, "educational intuition"<whatever that means, and outright pure guessing. That is bad enough, except as I state in the introduction to this blog, only about 28% of all mental health practitioners ever read any science. That means that the substantial majority of mental health practitioners are SCIENCE ILLITERATE, they might have well be totally illiterate because most of them probably can not read the eight grade level, and sure they can not do make any Critical Evaluation of Scientific Journals of their profession. To me that is shameful and not in the best interest of their patients. If you know anyone in mental health get an idea of what they know about science, for the most part they will not answer your questions or give you some horse rubbish that is not consistent with the truth.
Mental health practitioners like most persons in our society enjoy the benefits of science, but are ignorant of the science they enjoy. They can be bamboozle easily by their professors at the University that are just as likely to be science illiterate. Here is an article about what makes good science treatment.
There are numerous reasons why we get bamboozled into believing some mental health treatment and assessment are real and are valid and reliable. I will try to provide some educational information with references in the next few blog article. For thirty year the profession have been talking about "Evidence Based Treatment" (meaning based on scientific research). I have reason to believe that most practitioners haven't the faintest idea what Evidence Based means.
There are at least seven reasons why people may erroneously conclude that an ineffective therapy works:
Dr. Beyerstein, a member of the executive council of the Committee for Scientific Investigation of Claims of the Paranormal (CSICOP), is a biopsychologist at Simon Fraser University in Burnaby, British Columbia, Canada. A more detailed discussion of this topic is one of six superb articles on "alternative medicine" in the Sept/Oct 1997 issue of CSICOP's Skeptical Inquirer magazine, which costs $7.50. An introductory (six-issue) subscription at the special Internet price of $16.95 can be obtained by calling (800) 634-1610.
Mental health practitioners like most persons in our society enjoy the benefits of science, but are ignorant of the science they enjoy. They can be bamboozle easily by their professors at the University that are just as likely to be science illiterate. Here is an article about what makes good science treatment.
There are numerous reasons why we get bamboozled into believing some mental health treatment and assessment are real and are valid and reliable. I will try to provide some educational information with references in the next few blog article. For thirty year the profession have been talking about "Evidence Based Treatment" (meaning based on scientific research). I have reason to believe that most practitioners haven't the faintest idea what Evidence Based means.
Why Bogus Therapies Often Seem to Work
Barry L. Beyerstein, Ph.D.
Subtle forces can lead intelligent people (both patients and therapists) to think that a treatment has helped someone when it has not. This is true for new treatments in scientific medicine, as well as for nostrums in folk medicine, fringe practices in "alternative medicine," and the ministrations of faith healers.
Many dubious methods remain on the market primarily because satisfied customers offer testimonials to their worth. Essentially, these people say: "I tried it, and I got better, so it must be effective." The electronic and print media typically portray testimonials as valid evidence. But without proper testing, it is difficult or impossible to determine whether this is so.There are at least seven reasons why people may erroneously conclude that an ineffective therapy works:
1. The disease may have run its natural course. Many diseases are self-limiting. If the condition is not chronic or fatal, the body's own recuperative processes usually restore the sufferer to health. Thus, to demonstrate that a therapy is effective, its proponents must show that the number of patients listed as improved exceeds the number expected to recover without any treatment at all (or that they recover reliably faster than if left untreated). Without detailed records of successes and failures for a large enough number of patients with the same complaint, someone cannot legitimately claim to have exceeded the published norms for unaided recovery.
2. Many diseases are cyclical. Such conditions as arthritis, multiple sclerosis, allergies, and gastrointestinal problems normally have "ups and downs." Naturally, sufferers tend to seek therapy during the downturn of any given cycle. In this way, a bogus treatment will have repeated opportunities to coincide with upturns that would have happened anyway.
3. The placebo effect may be responsible. Through suggestion, belief, expectancy, cognitive reinterpretation, and diversion of attention, patients given biologically useless treatments often experience measurable relief. Some placebo responses produce actual changes in the physical condition; others are subjective changes that make patients feel better even though there has been no objective change in the underlying pathology.
4. People who hedge their bets credit the wrong thing. If improvement occurs after someone has had both "alternative" and science-based treatment, the fringe practice often gets a disproportionate share of the credit.
5. The original diagnosis or prognosis may have been incorrect. Scientifically trained physicians are not infallible. A mistaken diagnosis, followed by a trip to a shrine or an "alternative" healer, can lead to a glowing testimonial for curing a condition that would have resolved by itself. In other cases, the diagnosis may be correct but the time frame, which is inherently difficult to predict, might prove inaccurate.
6. Temporary mood improvement can be confused with cure. Alternative healers often have forceful, charismatic personalities. To the extent that patients are swept up by the messianic aspects of "alternative medicine," psychological uplift may ensue.
7. Psychological needs can distort what people perceive and do. Even when no objective improvement occurs, people with a strong psychological investment in "alternative medicine" can convince themselves they have been helped. According to cognitive dissonance theory, when experiences contradict existing attitudes, feelings, or knowledge, mental distress is produced. People tend to alleviate this discord by reinterpreting (distorting) the offending information. If no relief occurs after committing time, money, and "face" to an alternate course of treatment (and perhaps to the worldview of which it is a part), internal disharmony can result. Rather than admit to themselves or to others that their efforts have been a waste, many people find some redeeming value in the treatment. Core beliefs tend to be vigorously defended by warping perception and memory. Fringe practitioners and their clients are prone to misinterpret cues and remember things as they wish they had happened. They may be selective in what they recall, overestimating their apparent successes while ignoring, downplaying, or explaining away their failures. The scientific method evolved in large part to reduce the impact of this human penchant for jumping to congenial conclusions. In addition, people normally feel obligated to reciprocate when someone does them a good turn. Since most "alternative" therapists sincerely believe they are helping, it is only natural that patients would want to please them in return. Without patients necessarily realizing it, such obligations are sufficient to inflate their perception of how much benefit they have received.
Buyer Beware!
The job of distinguishing real from spurious causal relationships requires well designed studies and logical abstractions from large bodies of data. Many sources of error can mislead people who rely on intuition or informal reasoning to analyze complex events. Before agreeing to any kind of treatment, you should feel confident that it makes sense and has been scientifically validated through studies that control for placebo responses, compliance effects, and judgmental errors. You should be very wary if the "evidence" consists merely of testimonials, self-published pamphlets or books, or items from the popular media.Related Topics
- Spontaneous Remission and the Placebo Effect
- Common Questions about Science and "Alternative" Health Methods
- Why Extraordinary Claims Demand Extraordinary Proof
- How Quackery Sells
- Response to an Alt-Muddled Friend
Dr. Beyerstein, a member of the executive council of the Committee for Scientific Investigation of Claims of the Paranormal (CSICOP), is a biopsychologist at Simon Fraser University in Burnaby, British Columbia, Canada. A more detailed discussion of this topic is one of six superb articles on "alternative medicine" in the Sept/Oct 1997 issue of CSICOP's Skeptical Inquirer magazine, which costs $7.50. An introductory (six-issue) subscription at the special Internet price of $16.95 can be obtained by calling (800) 634-1610.
This article was posted on July 24, 2003.
Subscribe to:
Posts (Atom)